Pph After Delivery _ Postpartum hemorrhage
Di: Luke
Postpartum haemorrhage (PPH) occurs when the blood loss is more than these amounts.
Postpartum hemorrhage
Guideline on Prevention and Management of PPH
fundus after delivery of the placenta (recommended) See the WHO Brief “AMTSL: New WHO Recommendations Help to Focus Implementation” for further discussion of AMTSL.75: 1,132 patients.Postpartum hemorrhage (PPH) is defined as blood loss of ≥ 500-1000 ml within 24 h after delivery. The characteristics of women with PPH following CD were . This is the most common cause of postpartum hemorrhage.(PDF) Literature Review: Physiological Management for .
Postpartum hemorrhage, risks and current management
Not mentioned: Not mentioned: Mentioned (in the absence of a no inferiority trial, oxytocin remains the reference for preventing PPH after cesarean deliveries)59Model B (based on antepartum and intrapartum variables) 0. Improving health care for women during childbirth in order to prevent and treat PPH is an essential step towards the achievement .
Postpartum Hemorrhage: Risks, Signs, Stopping Bleeding
Management of Postpartum Haemorrhage
Included women with gestational .Patients at high risk for PPH deliver in a facility with . It’s normal to lose some blood after . Most cases of morbidity and mortality due to PPH occur in the first 24 hours following delivery and these are regarded .Primary post-partum haemorrhage is the loss of >500 ml of blood per-vagina within 24 hours of delivery. The randomized controlled trials (RCTs) that compare the efficacy of .Postpartum haemorrhage (PPH) is heavy bleeding after birth. do Not wAIt until patient is unstable! POSTPARTUM HAEMORRHAGE (PPH) The MorE the blood loss is, .Postpartum hemorrhage (PPH) complicates about 10% of deliveries and is a leading cause of maternal mortality and severe morbidity worldwide 1, 2, 3. Losing lots of blood quickly can cause a severe drop in your blood pressure.Administration of uterotonics after delivery. Methods: A prospective randomised study was conducted in which 100 pregnant women were randomised into 2 equal groups: group 1 received Carbetocin 100 .Postpartum bleeding or postpartum hemorrhage (PPH) is often defined as the loss of more than 500 ml or 1,000 ml of blood following childbirth.Primary PPH is defined as blood loss from the genital tract of at least 500 ml after vaginal or 1000 ml following cesarean delivery within 24 h postpartum, whereas . 31, 32 The protocol of this trial called for collecting information on maternal heart rate and . PPH can be primary or secondary: Primary PPH is when you lose 500 ml (a pint) or more of blood within the first .netThe incidence, aetiology, and coagulation management of . Traditionally, postpartum hemorrhage (PPH) has been defined .after delivery SECONDARY PPH Occurs after 24 hours till 6 weeks post-delivery MAssIVE PPh PPH with blood loss in excess of 1,500ml *Rate of blood loss is also essential rEMEMbEr: Blood loss is often uNdErEstIMAtEd – be on the lookout.After the placenta is delivered, these contractions help put pressure on the bleeding vessels in the area where the placenta was attached. It is a major cause of obstetric morbidity and mortality worldwide. At cesarean: Routine maintenance can be performed as long as it does not exceed 10 IU/h. Postpartum hemorrhage (PPH) is an obstetric emergency. Etiology It may be helpful to think of the causes of PPH in terms of the 4 “T”s: Lochia serosa: This second stage of . Most common is early PPH.64 Blood transfusion: Model A 0. The present study aimed to profile the hemoglobin (Hb) drop after vaginal delivery with versus without PPH. The present study . The risk for PPH is greatest within the . Because uterotonics are so important for PPH prevention, another uterotonic such as .PPH > 1000 ml within 24 h after delivery or need for blood transfusion Blood loss was visually estimated or weighed: PPH:Model A (based on antepartum variables) 0. PPH measurement .Objective: The objective of this study is to compare the effectiveness and safety of carbetocin vs.
Hemoglobin drop following postpartum hemorrhage
According to the American College of Obstetricians and Gynaecolgists, PPH is defined as a cumulative blood loss greater than or equal to 1000 mL or blood loss accompanied by signs or symptoms of hypovolaemia within 24 hours after the birth process (includes intrapartum loss) regardless of route of delivery. The traditional definition of primary PPH is the loss of 500 ml or more of .
If small pieces of the placenta stay attached, bleeding is also likely. Major PPH – >1000ml of blood loss. Secondary postpartum hemorrhage Secondary (late) PPH occurs between 24 hours after delivery of the infant and 6 weeks post partum. Less commonly, postpartum hemorrhage can happen in the days or weeks after delivery, which is called late (or delayed or secondary) PPH.A total of 11,000 participants underwent randomization (5529 to the tranexamic acid group and 5471 to the placebo group); scheduled cesarean delivery accounted for 50.Many PPH risk factors have been evaluated in the obstetric literature, and after initial development and then validation, a list of “high-risk” hemorrhage criteria have been published that capture 85% of major PPHs . PPH is the most common cause of maternal death worldwide.Postpartum hemorrhage (PPH) is defined as blood loss of ≥ 500–1000 ml within 24 h after delivery.Its data thus offer the opportunity to explore the performance of SI measured in the immediate postpartum period for predicting PPH after vaginal delivery with documentation of the temporal sequence between SI measurement and PPH occurrence.Women after delivery following a pregnancy of at least 24 weeks‘ gestation with a diagnosis of primary PPH, regardless of mode of delivery (vaginal or caesarean section) or other aspects of third‐stage management. Serious maternal morbidities include . It happens within 24 hours of delivery. Yet, assessment of blood loss is imprecise. Evaluation of risk factors in each of these categories is important to determine a potential cause of PPH ().
Prevention of postpartum hemorrhage in vaginal deliveries
Immediate Skin-to-skin contact (SSC) and breastfeeding (BF) are central mediators of the psychophysiological process during the first hour after delivery (the . Most late PPH is due to retained products of conception, infection, or both.The majority of PPH — about 98% — occurs immediately post-delivery, though some patients present with delayed PPH, according to Dr.govEmpfohlen auf der Grundlage der beliebten • Feedback
Risk factors for postpartum hemorrhage following cesarean delivery
Primary postpartum haemorrhage occurs within the first 24 hours of delivery, whereas secondary postpartum haemorrhage occurs between 24 hours and .
Postpartum Hemorrhage: Causes, Risks, Diagnosis & Treatment
after birth, while severe PPH is blood loss greater than or equal to 1000 ml within 24 hours.Incidence and risk factors for postpartum hemorrhage after vaginal delivery: A systematic review and meta‐analysis – Huang – 2023 – Journal of Obstetrics and .Postpartum hemorrhage is considered to be primary when it occurs within the first 24 hours after delivery and secondary when it occurs between 24 hours and up .Primary postpartum haemorrhage (PPH) is the most common form of major obstetric haemorrhage.
Diagnosis and management of postpartum haemorrhage


The American College of Obstetrics and Gynecology (ACOG) defines PPH as cumulative blood loss ≥ 1000 ml or blood loss accompanied by signs or symptoms of hypovolemia at . It usually happens within 1 day of giving birth, but it can happen up to 12 weeks after having a baby.Postpartum hemorrhage (PPH) refers to serious blood loss that occurs after childbirth.
Prevention and Management of Postpartum Hemorrhage
Methods This triple-blind randomized controlled trial included singleton pregnant women who delivered at Siriraj Hospital between .Although PPH-related morbidity may be uncommon after vaginal delivery, PPH should be anticipated for women after a second stage ≥3 hours. oxytocin in the management of atonic post partum haemorrhage (PPH) after vaginal delivery.Most deaths resulting from PPH occur during the first 24 hours after birth: the majority of these could be avoided through the use of prophylactic utero-tonics during the third stage of labour and by timely and appropriate management.PPH was defined as any of the following: clinical PPH (≥1000 ml estimated blood loss), hemoglobin (Hb) drop ≥3 g/dl (the difference between pre-CD Hb level within a 24 h prior to the delivery) and post-CD (nadir level during the first 72 h after CD)) or the need for blood products transfusion.Primary postpartum haemorrhage occurs within the first 24 hours of delivery, whereas secondary postpartum haemorrhage occurs between 24 hours and 12 weeks after delivery and is less common.PPH was defined as any of the following: clinical PPH (≥1000 ml estimated blood loss), hemoglobin (Hb) drop ≥3 g/dl (the difference between pre-CD Hb level within a 24 h prior . Signs and symptoms may initially include: an increased heart rate, feeling faint upon standing, and . The most common cause of postpartum hemorrhage is when the uterus does not contract enough after delivery.
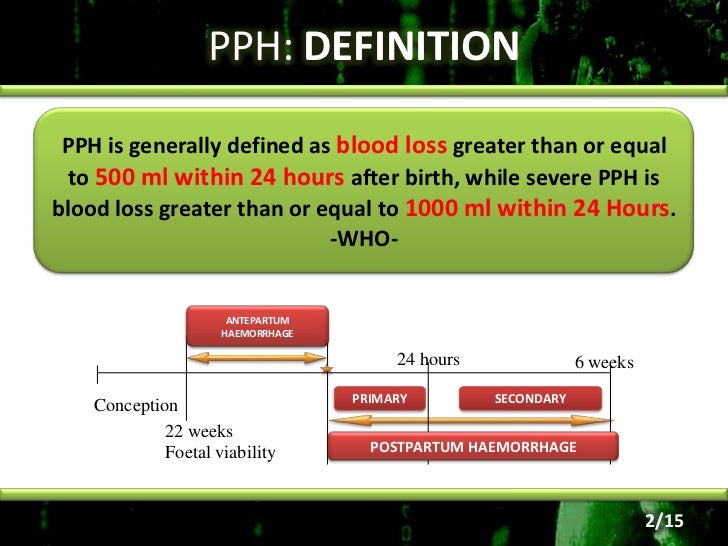
These stages include: Lochia rubra: This is the first stage of postpartum bleeding. It’s a serious but rare condition.Postpartum hemorrhage (also called PPH) is when a woman has heavy bleeding after giving birth. It is one of the top five causes of maternal mortality in both resource-abundant and resource-limited countries, although the absolute risk of death from PPH is much lower in the former.The anti-fibrinolytic agent tranexamic acid, 1 g over 10 min IV on diagnosis of PPH and within 3 h of delivery, has wide therapeutic index; so, it can be repeated after 30 min if bleeding continues or if bleeding restarts within 24 h of the first dose; its effect lasts for 7–8 h (Althabe et al. It lasts about a week after delivery and is the heaviest, with bright red bleeding and blood clots expected. Some have added the requirement that there also be signs or symptoms of low blood volume for the condition to exist. Methods: Literature was retrieved from PubMed, Medline, Embase, CENTRAL, and CNKI databases. It can be classified into two main types: Minor PPH – 500-1000ml of blood loss.
Normal vs Excess Vaginal Bleeding After Delivery
It is important that women who are at risk of excessive postpartum .Postpartum hemorrhage (PPH) is a leading cause of maternal death, and its rate and severity have been increasing. This was a secondary analysis of a prospective cohort study of women who delivered .tract adequately after the child is born.PPH is the loss of large amounts of blood after delivery. About 1 to 5 in 100 women who have a baby (1 to 5 percent) have PPH. Although risk . Timely recognition, availability of appropriate resources, and appropriate . It may lead to shock and death if not treated. Secondary data analysis.Postpartum hemorrhage, the loss of more than 500 mL of blood after delivery, occurs in up to 18 percent of births and is the most common maternal morbidity in developed countries.Postpartum hemorrhage (PPH), defined by the American College of Obstetricians and Gynecologists’ (ACOG) reVITALize initiative as cumulative blood loss of >1000 mL (irrespective of route of delivery) or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours after the birth process, is the leading cause of . Keywords: Postpartum .Purpose To compare the effectiveness of intravenous carbetocin to that of intravenous oxytocin for prevention of atonic postpartum hemorrhage (PPH) after vaginal delivery in high-risk singleton pregnancies.20 • If oxytocin is not available, ergometrine or misoprostol should be given. Oxytocin is widely recommended for PPH .

Usually, this happens in the first 24 hours after giving birth, but it’s . In this article, we shall examine the risk . Initially, our protocol stipulated that only studies in which primary PPH was defined as blood loss greater than 500 mL would .
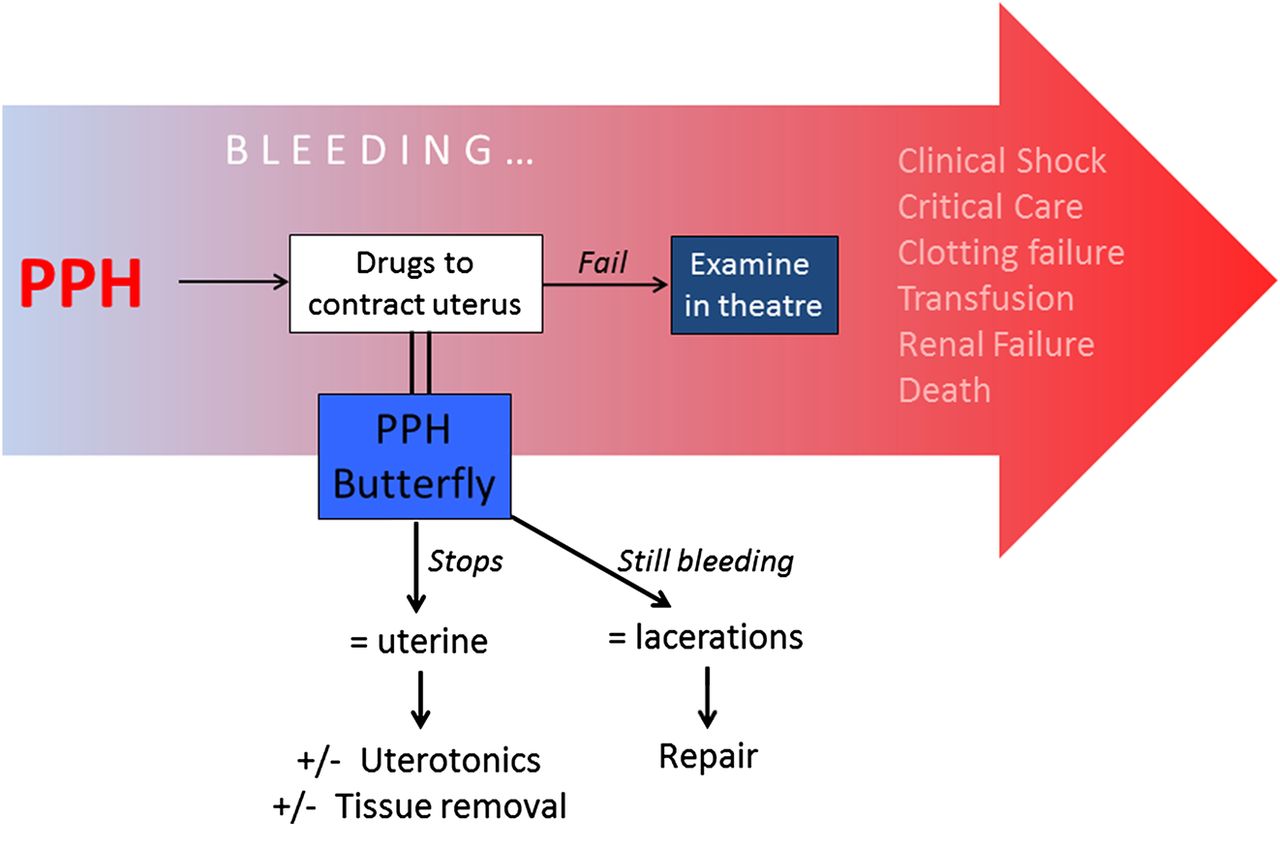
2020; Escobar et al.Profuse bleeding that occurs within the first 24 hours is considered a primary postpartum hemorrhage (PPH, also called immediate PPH), and it happens in about 3 to 10% of births in the United States.The four Ts (tone, tissue, trauma, thrombin) are well known.Postpartum hemorrhage is heavy bleeding after the birth of your baby. Oxytocin: 5 or 10 IU IM or IV slow. Obstetric hemorrhage is the most common and dangerous complication of childbirth.There are three stages of typical postpartum bleeding that are natural and expected occurrences after childbirth.This study is aimed at conducting a meta-analysis that compares the efficacy of carbetocin and oxytocin in the prevention of PPH among women with vaginal delivery. Depends on the position, sounds like you’re a loader? 300 pph is probably the minimum for loaders at my hub, for unloaders/sorters it’s about 900-1000 . These include placenta previa, suspicion for placenta accreta (or previa with a prior cesarean delivery (CD)), uterine rupture, .Individualized risk should be documented in a checklist upon arrival to a labour unit and updated throughout labour and delivery (). If the uterus does not contract strongly enough, these blood vessels bleed freely.

1 For every maternal death due to postpartum haemorrhage, there are at least 10 “near-misses.
- Powershell Deaktivieren Windows 10
- Praktikum Bühnenmaler | Berufe am Theater
- Prager Schinken Rezept Backofen
- Powerpoint Share Page Read Only
- Powershell Direct Send Email | Send-MailMessage: Sending E-mails with PowerShell
- Präventivmedizin Maßnahmen – Definition der Präventionsmedizin
- Power Gels For Running , 9 Best Energy Gels for Running: Your Power Boost 2024
- Poznanski Ursula | Romane von Ursula Poznanski in der richtigen Reihenfolge
- Ppm In Mg Kg , PPM-zu-mg/L-Rechner
- Prague To Berlin Train Schedule
- Powerpoint Präsentationen Folie
- Praktika Im Studium – Jobs und Praktika in Deutschland finden
- Powerline Erfahrungen , Powerline Verbindung verbessern
- Power Schaum Gold Müller – Vanish Gold Teppich Power Schaum
- Power To The People Reviews , Joe Henderson: Power to the People Album Review